Re-ramping Everyday Healthcare
Checklist for change
___________________________________________________
May 20, 2020
Throughout healthcare people are asking themselves How do I bring my patients back and re-engage in regular care? What does that look like in today’s COVID19 world? No matter how badly we all want normalcy, this next phase is not a return to our comfort zones and the way we did it 2 months ago. It’s time to create a new future.
After months of constant upheaval, re-engaging with patients at regular volumes hits us like another enormous communications and execution challenge. The rapid ramp-up of telehealth in a few weeks was just the beginning. Not surprisingly, there are gaps and glitches in the telehealth approach compared with how the telehealth roll-out might have gone if it had unfolded over the couple of years many planned or the 5 years some thought was more realistic.
- How we use Virtual Visits,
- How well we execute on all the necessary changes, and
- How responsive we are to patient needs in these difficult times … in short,
How we meet patients where they are, by updating and improving the patient experience, will drive how quickly patients return to everyday care.
Resource Planning and Execution Considerations
- What resources, if any, need diversion for treating and triaging COVID19?
- How do we maintain the safety of patients and clinical care teams?
- What additional safety steps need to happen?
- How do those necessary workflow adjustments affect our capacity?
- How much of both COVID19 and traditional care can be done by phone, video or alternate approach? e.g. Would vitals at the lab before a virtual visit with the doctor be more efficient than vitals at the doctor’s office?
- Once we make those adjustments, how much of our traditional capacity is lost?
- How can we plan creatively to make that up?
Communicating and Connecting with Patients
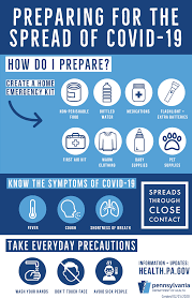
We all have overflowing inboxes and new demands on our time plus the constant stress of shelter in place. Patients are no different. They need specifics, and like us, patients want those specifics in an easy-to-digest format.
When communicating with patients, keep it short and actionable. Save broad messages for advertising. If necessary, we can target communications to smaller sub-groups of the patient community to increase relevance of information. Do Not send texts that say go to this website or call ### for more information. That is asking extra steps of stressed-out patients.
Key relevant points we should communicate directly
- Open with empathy – acknowledge that different patients will be comfortable with different tempos of re-ramping for normal healthcare interactions
- Clarify what is open when
- Provide a crisp outline of onsite safety protocols
- List additional and different steps for which the patient needs to plan
- Describe what we are doing to ease that burden
- Offer direct contact information - phone and email - for operational questions
Meet patients where they are by providing helpful information such as links to reliable, up-to-date sources of COVID19 information and easy ways to access the information and care they need now. Less helpful is pressing patients to search for answers on web sites or book now.
Challenge and Opportunity
Change is hard, in no small part because of all the extra work involved. Given current circumstance, there is no procrastinating this challenging work. The good news: it’s a great time to strengthen and update Doctor-Patient relationships. What can we improve while we are doing this work?
- Is timelier, more relevant Doctor-Patient dialogue possible if patient doesn’t have to go to the office?
- Do improved 2-way communication systems increase the likelihood that the doctor has lab results before a conversation?
- Increased patient flow with more patient-friendly scheduling systems
- Can we improve patient adherence by tapping systems used to coordinate off-site care?
Wish List?
Most of us in healthcare are already working on what the next phase looks like. Many of us were working on changes pre-Covid19. Now is a good time to review and revise our wish lists for opportunities to better leverage all this hard work and change.
On March 6, I was asked by a primary care practice what I thought of different patient portals. They were planning a change. At the time, I was inclined to emphasize the providers’ internal needs because pre-COVID19, most people I know wanted to use portals as little as possible (in their patient capacity😊 – conversation with Susannah Fox on this topic ). Today, I would prioritize patient ease of use above all other features because seamless 2-way communication is going to be essential going forward to meet patients where they are.
What are you wishing for near term?
Join in creating the future. Share your thoughts and priorities:
Critical Questions for Re-Thinking Healthcare

Covid-19 is a catalyst as well as a crisis. Personally, professionally and at broader levels of our communities, organizations and systems, we are re-thinking much of what we defined as “normal” a few, long weeks ago. Change at this speed is exhausting and can be overwhelming.
Breaking it down into phases helps me.
What Now?
It’s a simple imperative. #flattenthecurve so as not to overwhelm the healthcare system. Oh and prepare a health system, not designed for this, for a massive surge in demand. Simple to understand yet an enormous execution challenge that is overwhelming in its own right. Nonetheless we are doing it.
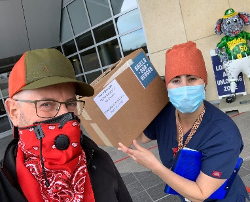
It’s awe-inspiring to watch people find their way to contribute. A college friend is re-purposing his small business resources to produce face shields for the front lines. Daily updates from @Bob_Wachter keep us informed and inspire others to share their local details and search for answers on what works best. My part seems to be connecting people and information across silos.
What Next?
We’ve all moved well beyond our traditional comfort zones. Moving forward will not be the same as going back to the way things were. As we gradually work to safely re-open the economy, we need to find new ways to get as close as possible to time-honored goals of traditional care delivery.
Despite the crisis Covid-19 is causing, it is a small piece of total health and wellbeing even now. Delaying medical care and the economic implications of Shelter-in-Place have their own life-threatening and quality-of-life implications. “Where have all the heart attacks gone?” and “What do I do about that upcoming well visit?” are both pressing questions that need short, as well as longer-term answers at both individual and community levels.
At the same time, we will still need surge capacity – the more mobile and flexible the better. It’s likely that outbreaks will continue to be a problem for a while, given the time it will take to develop vaccines, herd immunity and treatments. What does the Healthcare Covid-19 Surge Kit look like?
- How resource-efficient can we make it?
- How much of it can be shipped in?
- What parts have to be maintained locally?
- How much – or how little - of daily healthcare and life do we have to shut down to make it work?
- How do public and population health come together going forward?
What do we want going forward?
We’ve had no choice but to stretch and experiment. We are living through an unprecedented acceleration of change that has bent or ignored old rules where necessary, faced tough trade-offs and recalibrated our tolerance for risk. How can we leverage the learning from this historic shift to create a new, better era of healthcare?
- How can we improve public and population health by moving care closer to patients?
- How much of this solution will be telehealth and which part will be care in non-traditional settings like drive-through lab testing?
- How much efficiency and cost savings can we capture with a more flexible healthcare system? Can we use this increased flexibility to better serve the varying needs of time and place?
- Rural and underserved
- Home-based seniors
- Seasonal and local increases in demand
- How do we ease and speed adoption of new technologies such as telehealth, remote monitoring and tracking to facilitate quality care in more varied settings?
We’ve had much of the necessary technology for a long while. People’s ability to adapt and adopt has become the rate-limiting factor in transforming healthcare. Now that we’ve been forced into rapid and dramatic changes, how will we use the learnings and flexibility for sustainable positive change?
What do you think?
Please share your thoughts and critical questions with Kathryn.
Make change happen
Lots of great ideas in the latest Fixing Healthcare Podcast with Chip Heath. I will be listening again!
The discussion draws on the Heath brothers’ work to explain the HOW of connecting with people’s emotions to drive change and the science behind WHY these human approaches work.

It’s hard to pick a favorite. I was hooked at “shrink the change” because I think that is a big part of why our Stakeholder ΔApproach© works. And yet, the story of the gloves (near the end) calls to me the most because it was such a great way to make mountains of data come alive for the stakeholders who actually had to change focus and priorities to address a problem around which they did not feel pain today.
Highly recommend investing time in this. Would love to hear what your favorite nugget was? Let us know your thoughts in the comments here!
in·no·va·tion
/ˌinəˈvāSH(ə)n/
noun
New ways of achieving time honored goals
Beyond the Idea a quick read on executing innovation. We particularly like the emphasis on HOW to connect and cocoon innovation efforts in relation to the organization's traditional operations.